gastrointestinal surgeries
Gastrointestinal (GI) surgery encompasses a range of advanced surgical procedures performed on the digestive system, which includes the esophagus, stomach, small intestine, Large intestine (colon), rectum, liver, pancreas, gallbladder, and bile ducts. These surgeries are essential for diagnosing and treating various conditions affecting the GI tract, ranging from benign disorders to complex diseases.
Dr. Ajay Kumar Kriplani is a highly skilled specialist in gastrointestinal surgery, providing comprehensive care for patients dealing with a wide array of digestive conditions. With expertise in both minimally invasive laparoscopic techniques and traditional open surgery, Dr. Ajay Kumar Kriplani ensures precision, reduced recovery time, and optimal outcomes for every patient.
Hiatal Hernia and Gastro Esophageal Reflux Disease (GERD)
What is Hiatal Hernia?
A hiatus hernia is migration of the top part of the stomach or all of the stomach from its normal position in the abdomen, into the chest, through an opening in the diaphragm.
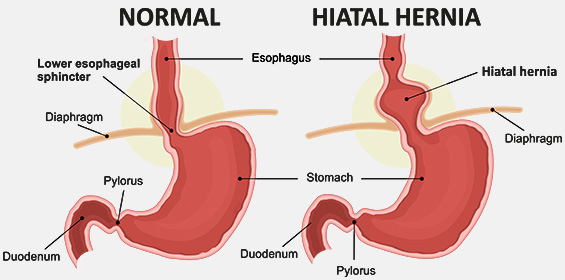
Diaphragm is the muscle that separates the abdominal cavity from the chest cavity. The food pipe (oesophagus) enters the abdomen from the chest through an opening in the diaphragm (esophageal hiatus) to connect to the stomach. This opening has to widen a little only to make a hiatal hernia possible. In Hiatus hernias, stomach slides up or pushes through the oesophageal hiatus opening. This is where the term, hiatus hernia, arises.
There is a natural one-way valve (lower oesophageal sphincter, LES) that allows food to pass from foodpipe into the stomach when we eat. After the bolus has passed, the LES tightens again and prevents acid / food reflux from the stomach into the oesophagus. Dysfunction / weakness of the valve leads to GERD. Hiatus Hernia disturbs the LES and allows acid to flow into the oesophagus.
What Causes Hiatus Hernia?
1. Increased pressure in the abdominal cavity that pushes the stomach upwards. This can happen while coughing, vomiting, straining during a bowel movement, exercising or lifting heavy objects. There are attachments that keep the oesophagus and stomach attached to the diaphragm, when these weaken; a hiatus hernia can form.
2. Age-related changes in the diaphragm. Hiatal hernias are most common in people who are age 50 years or obese.
3.Injury to the area, for example, after trauma or certain types of surgery.
What are the symptoms of Hiatus Hernia?
Unlike other hernias, Hiatus Hernia is not noticed as a bulge by the patient externally.
It doesn’t always cause symptoms, but when it does, they are usually related to acid reflux.
- Gastro-oesophageal reflux disease (GERD).
GERD occurs when stomach acids moves into the oesophagus (food pipe). Reflux of acid into the oesophagus can lead to- Heartburn: a feeling of burning in the chest that rises up from the stomach
- Burping and Regurgitation: stomach acid comes back up into the mouth with gas and food causing an unpleasant, sour taste.
- Pain when swallowing or difficulty swallowing. Most of the time, pain from a hiatal hernia is related to acid reflux rather
than the hernia itself. Acid irritates the foodpipe, which runs through chest up to throat. Pain may be felt higher or lower in the chest, or tradiate throughout the chest. It may even feel like a heart attack. The biggest difference is a heart attack usually feels like tightening and pressure in the chest, while heartburn feels more like burning. If in doubt, it is best to have chest pain checked by the doctor. - The lining of the foodpipe after prolonged exposure to acid gets inflamed (oesophagitis).
Chronic inflammation can cause ulcer formation Symptoms include painful swallowing, nausea and chest pain and rarely even gastro intestinal bleeding (black stools or blood in the vomitus).
- Oesophageal stricture. Chronic inflammation can cause scarring of the oesophagus tissues. Scar tissue makes the oesophagus narrow called stricture. This narrow area interferes with swallowing muscles and makes it hard to swallow.
- Barrett’s esophagus. Barrett’s oesophagus is tissue changes in the lining of the foodpipe, which can turn into cancer. About 5% to 10% of people with GERD develop this condition

Barrett’s oesophagus
- Hiatus Hernia can lead to more serious health problems depending on the amount of stomach that has migrated into the chest. This may lead to
- Chest discomfort after the meals and sometimes palpitation by pressure on the heart.
- Occasionally, the stomach gets twisted or folded on itself (gastric volvulus) and this is a surgical emergency
Investigations:- Upper GI endoscopy to look for extent of damage to food pipe lining (inflammation, ulcer and their extent, stricture, Barrett’s Oesophagus) and / or a hiatus hernia.
- Barium swallow: X rays after the patient swallows radio opaque contrast and images are taken to see the anatomy of the oesophagus and stomach. This may identify a hiatus hernia.
- 24 hrs. acid studies: 24hr pH studies, is a test for acidity within the oesophagus and the stomach. This is usually ordered to correlate the symptoms with acid reflux and is required particularly for atypical symptoms.
- Manometry: pressure testing of the oesophagus to check for the motility of the oesophagus. This helps to guide the surgical management.
- CT scan
Do hiatal hernias go away?
Hernias never go away. They usually get worse over time. If hiatal hernia is not causing any symptoms, it needs no treatment. But if it does, symptoms will continue and possibly worsen. Mild acid reflux may be managed with medications. More severe cases need surgical repair.
How is Hiatus Hernia Treatment?
- Medical treatment. Medications can reduce the acid content in the stomach. This makes reflux less damaging, allows time for the damaged esophageal tissue to heal and alleviates the pain associated with it. But they cannot stop acid reflux, regurgitation or stop hernia from growing.
Proton pump inhibitors (PPI) are commonly used, as they are stronger than H-2-receptor blockers. The medication generally needs to be continued for long term or lifelong.
The most common side effects of PPIs are mild and include Diarrhea, nausea, vomiting and stomach pain. PPIs may also raise chances of getting an infection of the intestines or lung but this is rare. These medicines have also been linked to fracture of the hip, wrist, and spine. The risk is highest in people who take PPIs for a year or more.
Along with medication, it is important to adopt some lifestyle changes for better symptom relief, which include
- Stop smoking and alcohol. They make symptoms worse.
- Lose extra weight.
- Foods. Certain foods and drinks should be avoided and include chocolates, coffee, caffeine, mint, fatty foods, Spicy foods, tomato sauce, garlic, onion etc. Some foods and drinks help with symptoms and may provide relief e.g. Chewing gum, Alkaline foods, including bananas, melons and cucumber, Baking soda mixed with water, Watery foods, like celery, lettuce and watermelon, Non-fat milk or yogurt, Ginger etc.
- Eat smaller portion size more frequently to reduce pressure in the stomach.
- Eat dinner early. Remain upright for at least two hour after eating befor going to bed.
- Elevate head end of the bed during night 6 to 8 inches and sleep on your left side to help prevent reflux.
- Look at the medicines. Use of anti-inflammatory and pain medicines (other than acetaminophen) contributes to heartburn.
- Surgery. Surgery corrects the hernia and prevents the reflux. Surgery is an option for anyone, though not everyone will need it. Some may need it sooner and others later. It is recommended for complications that medication cannot prevent or if medication causes side effect or the disease affects the quality of life. It is also recommended as an alternative to life long medications to avoid complications of long-term therapy and when the hernia is large enough to be a risk for major complications
LAPAROSCOPIC FUNDOPLICATION / HIATAL HERNIA REPAIR
Fundoplication and hiatal hernia repair are typically performed laparoscopically or with Robotic platform. The aim of the surgery is to reduce the hernia and bring the stomach back into its normal position in the abdomen and at the same time to improve the function of the LES (valve). Surgery involves dissection of the oesophageal hiatus (where the oesophagus passes through the diaphragm). The oesophagus is freed from its surrounding tissues so that 4-5cm of oesophagus comes easily within the abdomen. The hiatal opening is narrowed (hiatoplasty).
A fundoplication involves wrapping the fundus (part of the stomach) around the abdominal part of the oesophagus in a 360-degree manner (Nissen’s fundoplication) to help prevent reflux. Sometimes, hiatal hernia surgery is combined with weight-loss surgery, such as a sleeve gastrectomy.
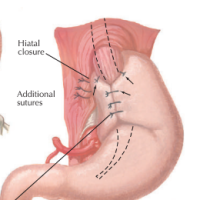
Nissen wrap
Recovery from hiatus hernia surgery
On the day of surgery, you will not be given any oral diet and you will continue to be on intravenous fluids. On the 1st post operative day, liquids will be started and after 48 hours generally you will be discharged. You can shower after 48 hours and climb stairs. You will continue to recover at home for another about 10 days. During the first week you will take liquids only due to temporary symptoms. Gradually progress to soft diet is made in the 2nd week. After 4 to 6 weeks you can expect to be back on normal diet.
Outcome after surgery for hiatus hernia
Hiatus hernia surgery gives 85 to 90% relief of symptoms. Most people are able to discontinue medications and enjoy life free of acid reflux after hiatal hernia surgery. Flatulance, some difficulty in swallowing and inability to belch are common and may slowly improve over months. You’ll have follow-up visits at least once a year after completing your recovery to check on your repaired hernia and make sure everything is still working right. A small percentage of hiatal hernias eventually return after surgery, usually after many years. This might be because the original forces that caused the first hernia are still active, and they caused a new one.
Risks
Occasionally, patients may have difficulty in swallowing after surgery. Endoscopic dilatation or further procedure may be required.
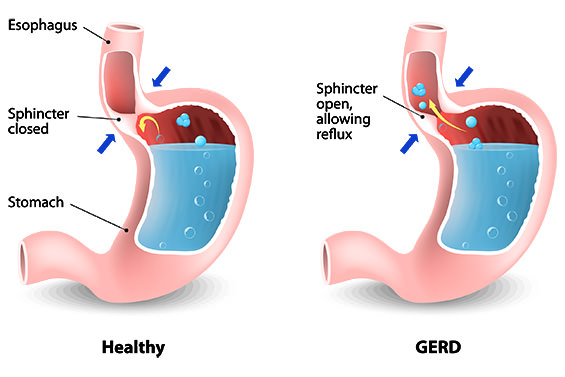
What REFLUX / GERD / HEARTBURN?
GERD is a very common condition. GERD frequently coexists with hiatus hernia and therefore these conditions are confused to be similar. Not all Hiatus hernias have GERD as symptoms and GERD may be present without a hiatus hernia.
Causes of GERD
There is a natural one-way valve (lower oesophageal sphincter, LES) that allows food to pass from foodpipe into the stomach but prevents acid / food reflux from the stomach into the oesophagus. Dysfunction / weakness of the valve leads to GORD. Factors that can affect this valve include:
Gastro Esophageal Reflux
- Hiatus Hernia:
- Oesophageal Dysmotility: normally the oesophagus propels food into the stomach in a progressive manner. When the oesophagus does not contract normally, this can lead to dysfunction of the LES.
- Obesity / increased BMI: excess fat in the abdominal cavity causes increase in the intra-abdominal pressure that leads to reflux. This increased pressure can also lead to a hiatus hernia.
Symptoms:
- Asymptomatic (no symptoms)
- GERD/regurgitation Gastro-oesophageal reflux disease (GERD) occurs when stomach acids moves into the oesophagus (food pipe). This causes heartburn/indigestion. After prolonged exposure to acid the lining of the foodpipe is damaged leading to ulcer formation, stricture (narrowing) and Barrett’s esophagus, which can turn into cancer.
Symptoms of GERD:
Reflux symptoms may be typical symptoms or atypical symptoms.
Typical symptoms:
- Heartburn: a feeling of burning in the chest that rises up from the stomach
- Regurgitation: stomach acids comes back up into the mouth causing an unpleasant, sour taste
- Pain when swallowing or difficulty swallowing
Atypical symptoms:
- Cough
- Hoarseness of voice
- Throat clearing, Dry sore throat
- Recurrent chest infections; pneumonia, asthma
- Ear pain
- Dental damage
- bad breath
Investigations:
- Upper GI Endoscopy
- 24 Hours Acid Studies
- Manometry
Treatment:
GERD is a very common condition, which is usually treated with lifestyle changes (stopping smoking, decreasing alcohol intake, avoiding spicy foods that trigger reflux and weight loss) and medications to reduce the acidity of the stomach. If symptoms are severe, laparoscopic surgery similar to hiatus hernia is used to treat GERD.
// click here for treatment
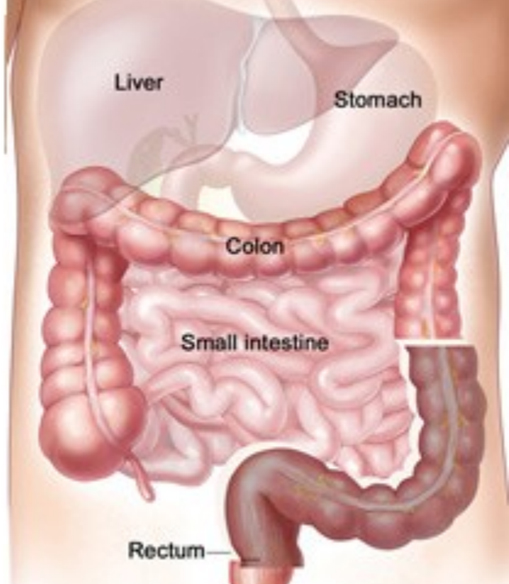
THE COLON
What is Colon?
The colon, also known as the large intestine, is a vital part of the digestive system. Colon, stretches from the end of the small intestines to anus. Various parts of the colon are shown in fig 1. Together, the small and large intestines measure about 27 feet with the colon making up the last 5 feet. Colon forms an inverted U-shape around the abdomen. Colon is three inches wide at its widest point, the cecum. It is just under an inch wide at its narrowest point, the sigmoid colon. Colons are host to trillions of microorganisms known as micro biota or gut flora. The majority of these organisms are bacteria.
By the time food reaches the colon most of the digestion process is complete. Colon is responsible for absorbing water and electrolytes, forming and storing faeces, and moving waste towards the rectum.
Common diseases of colon include irritable bowel syndrome (IBS), Colon tuberculosis, inflammatory bowel diseases (IBD) like Crohn’s disease and ulcerative colitis, diverticulitis, colon polyps and colorectal cancer.
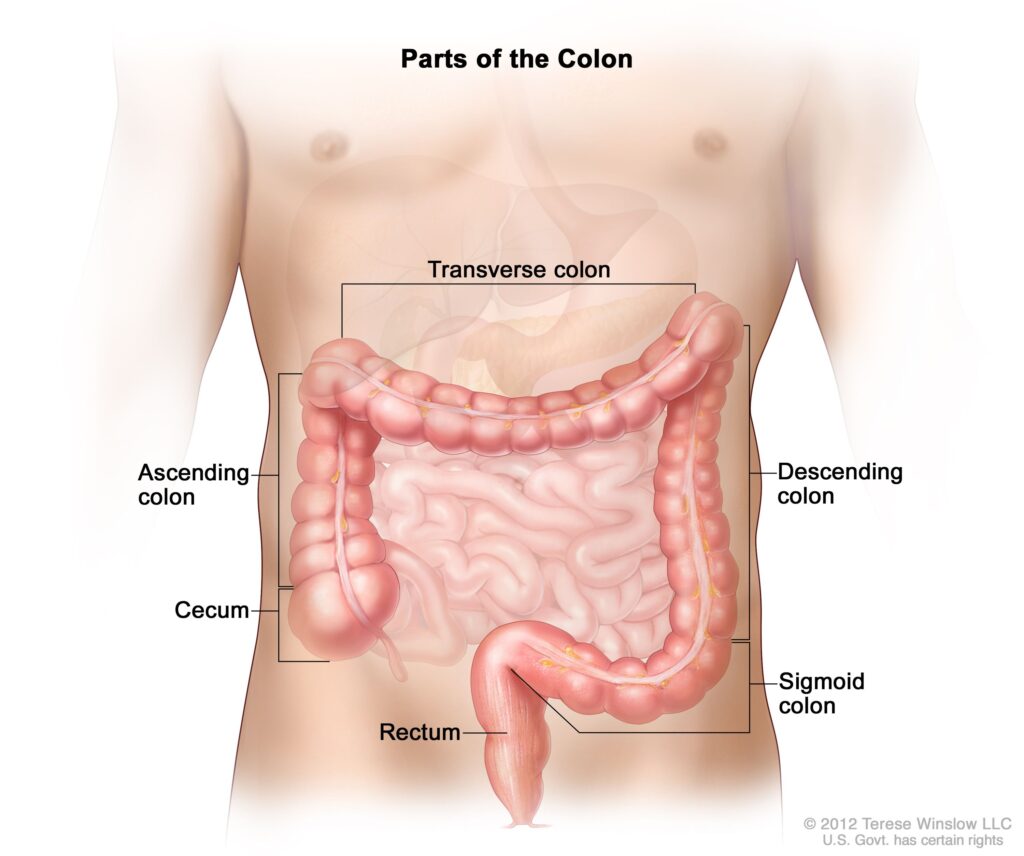
Fig. 1
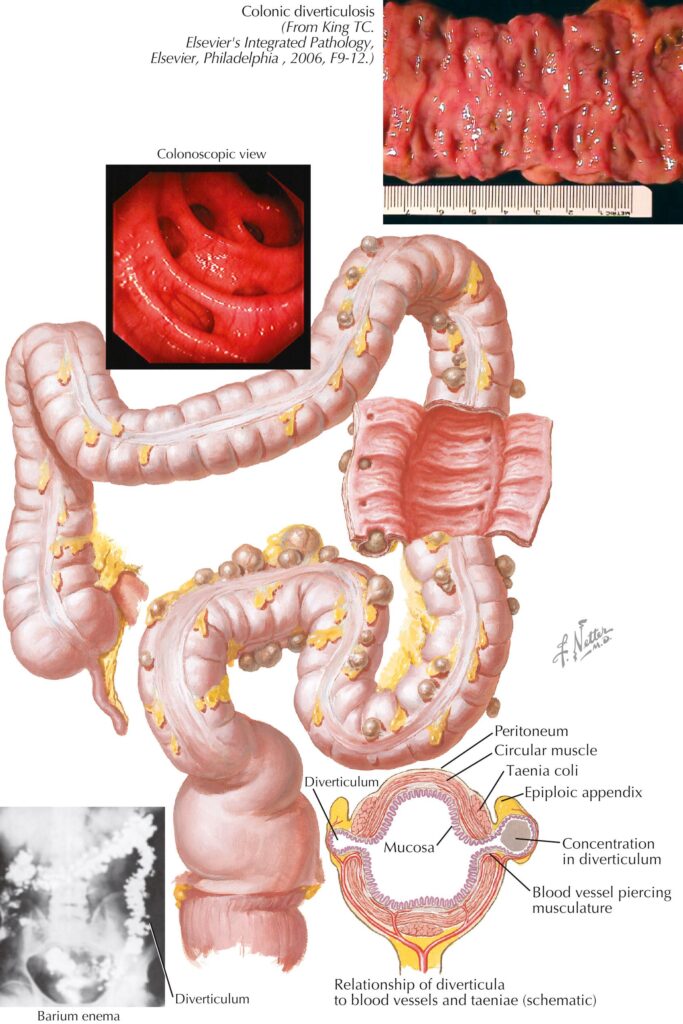
DIVERTICULOSIS AND DIVERTICULITIS
What are diverticulosis and diverticulitis?
Diverticulosis is a condition characterized by the presence of small, bulging pouches or pockets (diverticulae) in the lining of the large intestine (colon) (Fig diverticulosis photoshop). Diverticulosis can occur in any part of the colon but they are more common tin the distal part (sigmoid) of the colon though in Asia the first part (caecum) is also frequently affected. Diverticula can become inflamed or infected when stool or other material gets trapped, a condition known as diverticulitis.
WHAT ARE THE CAUSES OF DIVERTICULOSIS AND DIVERTICULITIS?
Diet plays a very important role. Diet low in fiber and high in refined foods may increase the risk. Lack of fiber leads to increased bowel wall strain to move stool through the colon. which increases local pressures that lead to the formation of pouches at weak points in the colon wall. With low fibre diet, resultant constipation and straining during stools may create enough pressure in the intestinal walls to cause diverticula.
Aging and heredity are other factors in the development of diverticulosis and diverticulitis, Incidence of diverticulosis increases with age. Diverticulitis will occur in about 10%-25% of those with diverticulosis.
The increased pressure along with undigested food caught in these pouches can erode the diverticular wall, causing inflammation and possible bacterial infection, which can result in diverticulitis.
WHAT ARE THE SYMPTOMS OF DIVERTICULOSIS?
Asymptomatic: Many patients may not have symptoms from diverticulosis alone. It is noticed due to tests done for some other condition.
- Pain lower abdomen. Pain is often crampy, and it comes and goes. The pain is commonly focused in the left side of the abdomen (belly) where the diverticula most often occur. Pain and bloating can often start after food is eaten and may ease when a stool or wind is passed.
- Altered bowel habits. Many people experience a change with diarrhea one day and constipation the next.
- Diverticular bleeding. This can happen if hard stool passing through a diverticulum erodes or stretches a blood vessel until it breaks. It is usually temporary and painless, but if it happens, there will be fresh blood in the stools. Sometime the bleeding may be serious.
If there is bleeding, persistent symptoms or complications from diverticulosis, it’s called “diverticular disease”. BOUT TRANSCRIPT
Symptoms of diverticular disease may overlap with conditions such as irritable bowel syndrome (IBS), colitis and cancer.
WHAT ARE THE COMPLICATIONS OF DIVERTICULOSIS?
Diverticulitis can cause life-threatening complications such as
- Inflammation (Diverticulitis): This is the most common complication, occurring among 1 in 10 persons with diverticulosis. Inflammation and/or infection occur because of an overgrowth of bacteria in the diverticula. Symptoms of diverticulitis include
Worsening abdominal pain.
High temperature.
Nausea / vomiting
If any of these symptoms are experienced, medical help should be sought immediately. Sometimes, when infection is severe, it can cause further complications such as: - Perforation. The weak lining of the diverticula which has no support breaks down causing a hole in the wall of the colon with resultant leakage of colon content full of bacteria into the abdominal (peritonitis) with spread of infection or leading to
- Abscess (collection of pus) around the colon when body tries to contain the infection.
- Obstruction (blockage of the bowel) may develop with the colon becoming rigid and scarred with thick wall and narrow lumen (Fig 2).
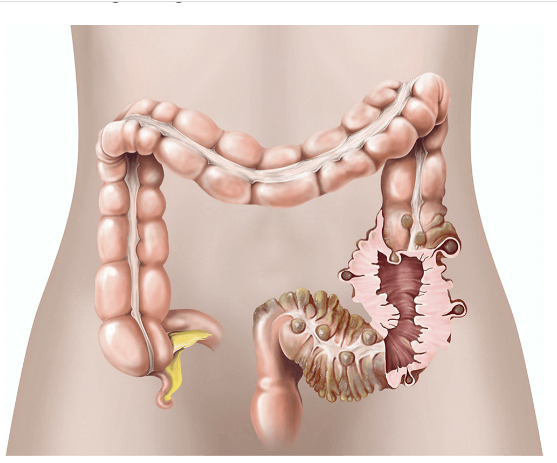
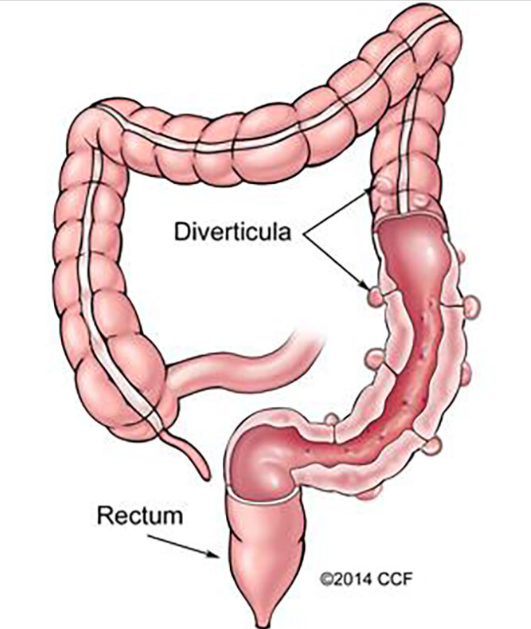
Fig 2
- Fistulas: Rarely, diverticula may lead to formation of abnormal connections or tracts (fistulas) between the colon and other organs such as the urinary bladder or vagina. Signs of this include small amounts of stool in the urine or foul-smelling discharge from the vagina.
HOW ARE DIVERTICULOSIS AND DIVERTICULITIS DIAGNOSED?
The tests may include:
- Colonoscopy A flexible tube with a camera at the end is used to look insides of the colon and rectum. It is an outdoor procedure performed under sedation. Medicines are prescribed the day before to cause diarrhea. This ensures empty bowels for inspection. It is a good idea to stay near a toilet. Note is made of location and distribution of diverticula which helps in assessing the area of colon involved and planning the extent of resection,
- A CT scan is a noninvasive, X ray based test, which makes images of the digestive tract. This test is more useful during an acute attack when colonoscopy is not preferred. This test also reveals any abscess, thickening of colon wall and narrowing.
- A lower GI series uses X-rays to get a better look at large intestine particularly strictures of the colon.
- Virtual colonoscopy. This is a CT scan that checks the colon using air and
- A blood sample shows signs like anemia or inflammation.
WHAT ARE THE TREATMENTS FOR DIVERTICULOSIS AND DIVERTICULITIS?
Once diverticulae develop, they are there to stay unless surgically removed. Not all diveticula need surgical removal.
- Diet Modification. Chances of developing an infection can be minimised by eating high fibre diet such as
- Whole-grain breads, cereals, and other items
- Fruit, such as apples, peaches and berries,
- Vegetables, such as broccoli, cabbage, spinach, carrots, asparagus, and squash
High fibre diet ensures the bowels move regularly and reduces the odds of getting diverticulitis. Diverticulosis patients should drink a lot of water (2 liters per day) daily to prevent constipation. Fat slows down the passage of food through the intestine hence low fat diet should be taken. Yogurt and supplements are good sources of probiotics. Nuts, seeds like sunflower, and even little seeds in fruits and vegetables such as cucumbers and strawberries don’t harm people with diverticulosis.
- Mild inflammation is treated by bed rest, diet modifications (liquid fiet) and, antibiotics to fight infection, antispasmodic drugs and possibly surgery.
- A more severe infection or perforation requires hospitalisation with intravenous (through a vein) fluids to give rest to the inflamed diverticula, nil by mouth and intravenous antibiotics
In addition, infected abscesses may require percutaneous drainage (a tube placed under the guidance of ultrasound or CT scan to take out the pus) and sometims performing a temporary colostomy to give the intestinal tract rest . The proximal colon is brought up to the skin and an opening made so as the bowel contents come into the bag rather than going to the colon. Diverting the faecal stream decrease leakage and gives the inflammed colon time to heal.
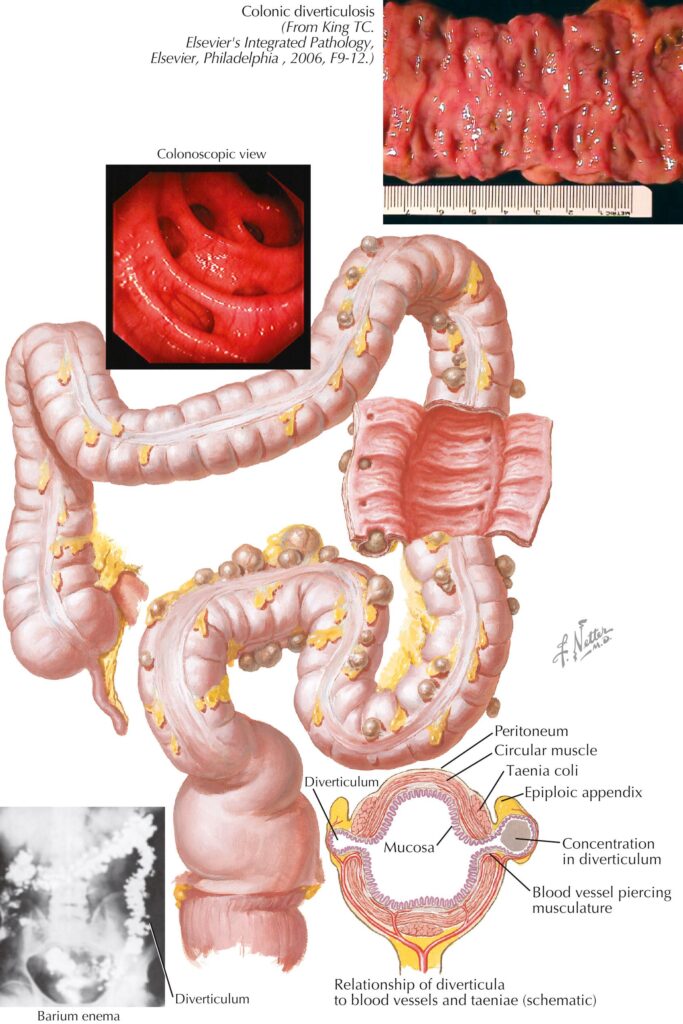
Fig diverticulosis photoshop
Surgery:
If multiple attacks of acute diverticulitis affects quality of life or after serious complications (perforation, abscess, G I bleed), it is recommended t to remove the affected section of the colon.Since in majority of patient diverticulae are in the left lower colon, the procedure is sigmoid colectomy (Fig 3). The surgery is preferrably done electively when the acute event has subsided so that the anastomosis heals properly. This prevent srecurrent life threatening complicatios.
Types of Diverticulitis Surgery
Resection and anastomosis
In this procedure, the surgeon removes the diseased portion of the intestine and reconnects the healthy areas. In more mild cases, this surgery can be performed using less invasive laparoscopic or Robotic techniques. This type of resection is often used in non-emergency cases.
Resection & Colostomy
If the intestinal inflammation is too great, after removing the diseased portion, it may not be safe to reconnect the end of the colon to the rectum because inflammation / infection compromises healing and chances of leakage of the anastomosis is high. In such a situation after the segment of the bowel with the infected pockets is cut and removed a colostomy is created. Proximal end of the colon is brought up to the skin as a stoma. Waste flows through the opening and collects in a bag.
After a few months, once the inflammation has reduced, colostomy is reversed. the colon is surgically reconnected so that faeces flow normally through the rectum. The stoma is closed and colostomy bag removed.
What are the benefits of surgery?
Relief from symptoms that are caused by diverticular disease and improvement in the quality of life.
Are there any alternatives to surgery?
Mild to moderate diverticular disease may be treated with repeated courses of antibiotics and increasing the amount of fibre in the diet may help but the diverticulae will not get better.
If complications have occurred (peforation, abscess, obstruction or a fistula), it will probably not heal without surgery.
Bleeding:
Where a severe bleeding episode has occurred an emergency blood transfusion may be required. Bleeding stops in 8 in 10 patients. In a a severe bleeding episode, various endoscope techniques can also be used. Alternatively, an angiogram can locate the bleeding vessel which is then treated by injecting medications into the blood vessel.
CANCER OF THE COLON
What is Camcer of the Colon?
Most colon cancers start as a polyp that subsequently undergoes transformation into cancer. Hereditary colon cancer accounts for about 5% of colon cancer when certain gene mutations are passed down from the parents.
Different types of colon cancer are found in different areas. Most colon cancer is adenocarcinoma. It is found in the inner lining of the colon. Less common types include Carcinoid tumors, which produce hormones, gastrointestinal stromal tumors (GIST) found in soft tissues and lymphoma (lymph nodes).
HOW IS COLON CANCER DIAGNOSED?
- Colonoscopy. A long, flexible tube with a camera is placed to check the insides of the colon for any cancers or growths that could turn into cancer. If polyps are found they are removed during the procedure. Most polyps are not cancerous though most colon cancers start as a polyp.
- MRI or CT scan may be done to confirm the location, extent and spread of the disease within the colon and outside in the Pelvis / abdomen (staging).
- PET CT when spread outside the abdomen is suspected.
- Blood tests to detect Anaemia, liver functions and CEA (a tumor marker that is helpful in the follow up as an indicator of recurrence).
WHAT ARE COLORECTAL CANCER TREATMENTS?
Prompt treatment for colon cancer is the best chance for recovery. The treatment of colorectal cancer depends on the size of the tumor, its location and “stage” of the disease.
A malignant pedunculated polyp (with a stalk) may be removed by colonoscopy (polypectomy) and the base examined for evidence of cancer cells.
SURGERY FOR COLORECTAL CANCERS
Surgery is considered the best choice for colon cancers stages 1 to 3. For sessile (without stalk) / larger tumors, surgery is required to take out the diseased part of the colon alongwith its draining lymph nodes (Fig) and
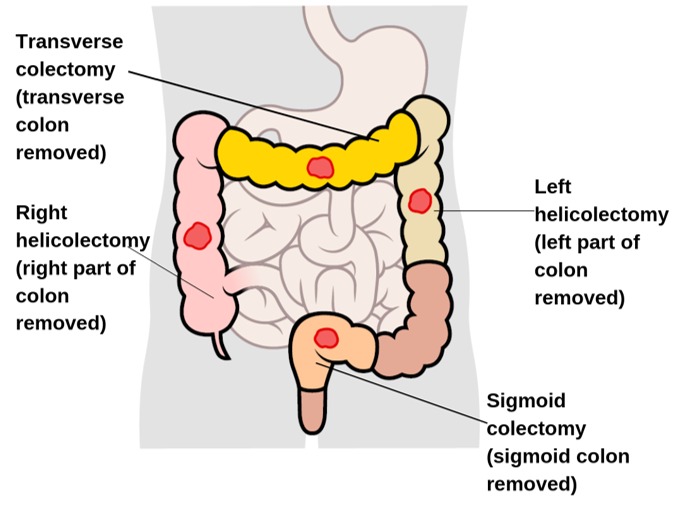
reattach the healthy tissue so that bowel continuity is maintained. This is called Colectomy and anastomosis. Depending on the location of tumor it may be right hemi colectomy, transverse colectomy, left hemi colectomy, sigmoid colectomy, anterior resection or low anterior resection.
In stage IV tumors (when tumor has spread to distant organs like liver, lings, brain, bones), also known as metastatic cancer, chemotherapy is the main treatment.
Surgery to bypass the cancer and connect the healthy parts of the colon may be required even in stage IV disease in the presence of obstruction. Alternatively a stoma may be formed where the colon proximal to obstruction is brought up to the skin and allowed to drain in a bag on the abdominal wall. Stoma or bypass Surgery can relieve or avoid blockage of the rectum or treat bleeding that is otherwise hard to control. It is not a cure, though it may help prolong life and improve quality of life.
Chemotherapy may be added depending on the MRI or histopathology report before or after surgery for rectal and anal canal tumors.
COLON CANCER VS. RECTAL CANCER
When cancer is found in the last 20 centimeters of the colon, it’s called rectal cancer. Rectal cancers are more aggressive than colon cancers. Radiation therapy / Chemotherapy may be recommend before surgery. Radiation can shrink the size of the lesion and lead to a better surgical result.Radiation may be considered after surgery to make sure no tumor is left behind.
WHAT ARE THE VARIOUS APPROACHES TO COLON CANCER SURGERY?
- Open surgery: In the more conventional approach,
- through a long incision in the abdomen, colon is accessed and the affected part is removed which include the cancerous tissue along with the lymph nodes to assess the spread of the cancer.
- Minimally invasive surgery: In this newer approach, laparoscopic technique or robotic technology (a robot is guided by the surgeon to dosurgery) is used to perform the surgery and achieve the same goal. The surgeon makes multiple small cuts in the skin of the belly. A tiny video camera is placed into one of the cuts to see inside the body. With the use of long, thin tools put into the other cuts the surgery is performed.
With minimally invasive procedures, patients experience:
- Less pain (and less need for pain medications)
- Less time at the hospital
- A shorter recovery, allowing them to get back to work and everyday activities more quickly
- Fewer (and less severe) side effects after pelvic surgery e.g. lesser disturbances with Bladder function, Bowel movement frequency and Sexual function
Our team has perfected these techniques and can perform these complex surgeries in less invasive ways.
A colostomy for a short time may be required to let the colon heal after surgery, which is closed by a second procedure after a few months.
WHAT ARE THE RISKS OF A COLECTOMY?
Some common risks for a colectomy are:
- Bleeding
- Damage to nearby organs
- Leaking where the intestines are attached together
- Infection at the incision or inside the belly
HOW LONG THE COLON CANCER WAS PRESENT WITHOUT KNOWING?
Symptoms during the early stages of colon cancer can go unnoticed for many years, as some cancers start as polyp that later become harmful.
WHAT IS THE LIFE EXPECTANCY OF SOMEONE WITH COLORECTAL CANCER?
The prognosis for colon cancer depends on which stage the cancer is diagnosed. Colon cancers in early stages have a good prognosis with nearly 90% of patients going 5 years and beyond, enjoying normal health. If the disease has spread to nearby lymph nodes, the figures are still a good 72%. However if it spreads to distant organs or farther lymph nodes, the figure drops to 13%. For all stages of colon cancer combined, the 5-year survival rate is about 63%.
Treatment for colon cancer can be successful in cases where the cancer has only spread to one or a few spots in the liver or lungs. In these cases, surgery can increase life expectancy and possibly cure the cancer.
Symptoms of Colorectal Cancer
The symptoms of colon cancer can vary, depending on the location of the tumor.
- Bleeding. It is one of the early symptoms. Often, bleeding in the stools may be only small amounts and off and on. Many other conditions can cause blood in the stools that include haemorrhoids, ulcers, polyps, colitis, inflammatory bowel diseases etc. A surgeon must be immediately consulted to find out the cause and source of blood in the stools.
- Change in bowel habits is common. Constipation or alternating constipation and diarrhea may be present in colorectal cancer. This is more common in left sided or larger cancers.
- Unexplained Anaemia. Anaemia is shortage of RBCs in the blood and occurs due to loss of blood in the stools. It is more common in right-sided colonic cancers.
- Unexplained weight loss.
- Fatigue
- Pelvic Pain, Unusual stomach or gas pain.
If any of these symptoms are noticed, it is important to see the surgeon to ensure proper diagnosis and treatment. For a patient with colorectal cancer, early diagnosis and treatment can be a lifesaver.
HOW IS COLON CANCER DIAGNOSED?
- Colonoscopy. A long, flexible tube with a camera is placed to check the insides of the colon for any cancers or growths that could turn into cancer. If polyps are found they are removed during the procedure. Most polyps are not cancerous though most colon cancers start as a polyp.
- MRI or CT scan may be done to confirm the location, extent and spread of the disease within the colon and outside in the Pelvis / abdomen (staging).
- PET CT when spread outside the abdomen is suspected.
- Blood tests to detect Anaemia, liver functions and CEA (a tumor marker that is helpful in the follow up as an indicator of recurrence).
WHAT ARE COLORECTAL CANCER TREATMENTS?
Prompt treatment for colon cancer is the best chance for recovery. The treatment of colorectal cancer depends on the size of the tumor, its location and “stage” of the disease.
A malignant pedunculated polyp (with a stalk) may be removed by colonoscopy (polypectomy) and the base examined for evidence of cancer cells.
SURGERY FOR COLORECTAL CANCERS
Surgery is considered the best choice for colon cancers stages 1 to 3. For sessile (without stalk) / larger tumors, surgery is required to take out the diseased part of the colon alongwith its draining lymph nodes (Fig) and
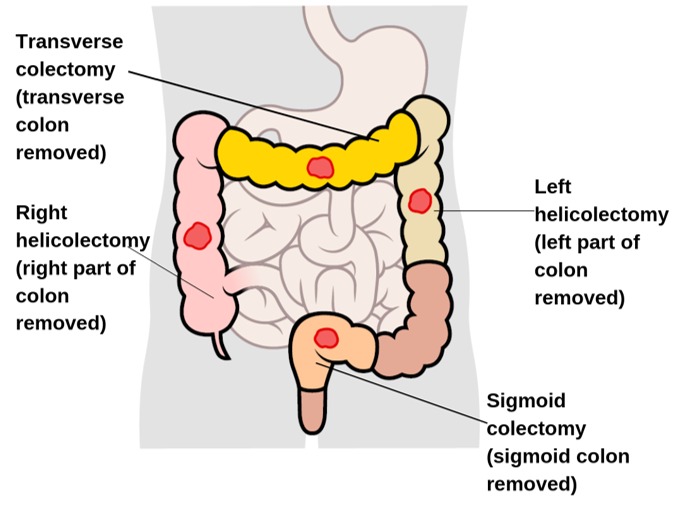
reattach the healthy tissue so that bowel continuity is maintained. This is called Colectomy and anastomosis. Depending on the location of tumor it may be right hemi colectomy, transverse colectomy, left hemi colectomy, sigmoid colectomy, anterior resection or low anterior resection.
In stage IV tumors (when tumor has spread to distant organs like liver, lings, brain, bones), also known as metastatic cancer, chemotherapy is the main treatment.
Surgery to bypass the cancer and connect the healthy parts of the colon may be required even in stage IV disease in the presence of obstruction. Alternatively a stoma may be formed where the colon proximal to obstruction is brought up to the skin and allowed to drain in a bag on the abdominal wall. Stoma or bypass Surgery can relieve or avoid blockage of the rectum or treat bleeding that is otherwise hard to control. It is not a cure, though it may help prolong life and improve quality of life.
Chemotherapy may be added depending on the MRI or histopathology report before or after surgery for rectal and anal canal tumors.
COLON CANCER VS. RECTAL CANCER
When cancer is found in the last 20 centimeters of the colon, it’s called rectal cancer. Rectal cancers are more aggressive than colon cancers. Radiation therapy / Chemotherapy may be recommend before surgery. Radiation can shrink the size of the lesion and lead to a better surgical result.Radiation may be considered after surgery to make sure no tumor is left behind.
WHAT ARE THE VARIOUS APPROACHES TO COLON CANCER SURGERY?
- Open surgery: In the more conventional approach,
- through a long incision in the abdomen, colon is accessed and the affected part is removed which include the cancerous tissue along with the lymph nodes to assess the spread of the cancer.
- Minimally invasive surgery: In this newer approach, laparoscopic technique or robotic technology (a robot is guided by the surgeon to dosurgery) is used to perform the surgery and achieve the same goal. The surgeon makes multiple small cuts in the skin of the belly. A tiny video camera is placed into one of the cuts to see inside the body. With the use of long, thin tools put into the other cuts the surgery is performed.
With minimally invasive procedures, patients experience:
- Less pain (and less need for pain medications)
- Less time at the hospital
- A shorter recovery, allowing them to get back to work and everyday activities more quickly
- Fewer (and less severe) side effects after pelvic surgery e.g. lesser disturbances with Bladder function, Bowel movement frequency and Sexual function
Our team has perfected these techniques and can perform these complex surgeries in less invasive ways.
A colostomy for a short time may be required to let the colon heal after surgery, which is closed by a second procedure after a few months.
WHAT ARE THE RISKS OF A COLECTOMY?
Some common risks for a colectomy are:
- Bleeding
- Damage to nearby organs
- Leaking where the intestines are attached together
- Infection at the incision or inside the belly
HOW LONG THE COLON CANCER WAS PRESENT WITHOUT KNOWING?
Symptoms during the early stages of colon cancer can go unnoticed for many years, as some cancers start as polyp that later become harmful.
WHAT IS THE LIFE EXPECTANCY OF SOMEONE WITH COLORECTAL CANCER?
The prognosis for colon cancer depends on which stage the cancer is diagnosed. Colon cancers in early stages have a good prognosis with nearly 90% of patients going 5 years and beyond, enjoying normal health. If the disease has spread to nearby lymph nodes, the figures are still a good 72%. However if it spreads to distant organs or farther lymph nodes, the figure drops to 13%. For all stages of colon cancer combined, the 5-year survival rate is about 63%.
Treatment for colon cancer can be successful in cases where the cancer has only spread to one or a few spots in the liver or lungs. In these cases, surgery can increase life expectancy and possibly cure the cancer.
What Are the Causes of Diverticulosis and Diverticulitis?
Aging and heredity are primary factors in the development of diverticulosis and diverticulitis, but what you eat also plays a role. Eating a diet low in fiber and high in refined foods may increase the risk. Indeed, in Western societies, an estimated 10% of people over 40 develop diverticulosis; the figure reaches at least 50% in people over 60. Diverticulitis will occur in about 10%-25% of those with diverticulosis.
Though it hasn’t been proven, some researchers think that if you are often constipated and usually strain when you have a bowel movement, you may create enough pressure in the intestinal walls to weaken them and begin the development of diverticular pouches. Another school of thought is that not enough fiber in the diet is responsible. The lack of fiber leads to increased bowel wall strain to move stool through the colon. That then causes increased local pressures that lead to the formation of pouches at weak points in the colon wall. The increased pressure along with undigested food caught in these pouches can erode the diverticular wall, causing inflammation and possible bacterial infection, which can result in diverticulitis.
HOW ARE DIVERTICULOSIS AND DIVERTICULITIS DIAGNOSED?
Most doctors don’t notice cases of diverticulosis until they screen for other conditions. For instance, the pouches might show up in a colonoscopy or an X-ray.
Your doctor might take these steps to know for sure:
Gather your medical history. They’ll ask you about your diet, general health, meds you take, and how often you have bowel movements.
Do a physical exam. This may include a digital rectal exam. With a lubricated gloved finger, they’ll gently check your anus for bleeding, pain, or other signs.
Perform tests. These might include:
- A CT scan makes images of your digestive tract.
- A colonoscopy looks in your rectum and colon.
- A blood sample shows if you have signs like anemia or inflammation.
- A lower GI series uses X-rays to get a better look at your large intestine.
WHAT ARE THE TREATMENTS FOR DIVERTICULOSIS AND DIVERTICULITIS?
Once you develop diverticula, they are there to stay unless you have them surgically removed, which is not usually done. You can minimize the chances of developing an infection by modifying your diet. If you have a mild case of diverticulosis, your doctor may have you eat a high-fiber diet to make sure the bowels move regularly and to reduce the odds of getting diverticulitis.
Barium Enema: What to Expect Before and After the Test
If you develop diverticulitis you need to see a doctor to make sure you recover completely and to avoid possible life-threatening complications. Diverticulitis is treated using diet modifications, antibiotics, and possibly surgery.
Mild diverticulitis infection may be treated with bed rest, stool softeners, a liquid diet, antibiotics to fight the infection, and possibly antispasmodic drugs.
However, if you have had a perforation or develop a more severe infection, you will probably be hospitalized so you can receive intravenous (through a vein) antibiotics. You may also be fed intravenously to give the colon time to recuperate. In addition, your doctor may want to drain infected abscesses and give the intestinal tract a rest by performing a temporary colostomy. A colostomy creates an opening (called a stoma) so your intestine will empty into a bag that is attached to the front of the abdomen. Depending on the success of recovery, this procedure may be reversed during a second operation.
If you have several attacks of acute diverticulitis, your doctor may want to remove the affected section of the intestine when you are free of symptoms. You may also need surgery if intravenous therapy does not effectively treat an acute attack of diverticulitis. Whatever the treatment, the chances for a full recovery are very good if you receive prompt medical attention.
DIVERTICULITIS AND DIVERTICULOSIS DIET
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
WHAT CONDITIONS CAN ROBOTIC SURGERY TREAT?
Robotic surgery is used to treat a wide range of surgical conditions. It is especially helpful for
Abdominal wall Hernia It avoids use of stapler to fix the mesh in hernia and hence causes less pain.
Hiatus hernia and Achalasia. Robotic surgery is helpful as gives more magnified and in depth view of the hiatus.
Bariatric surgery: Sleeve gastrectomy and Gastric bypass roux en Y. Robotic view is superior to laparoscopic view.
Colon and rectum surgery
Biliary tract including gall bladder removal
Oesophagus, stomach, liver and pancreas and
Oher complex surgeries.
TECHNOLOGY BREAKTHROUGHS
Many hospitals around the globe now use robotic surgery to treat a broad spectrum of medical conditions. More and more hospitals are acquiring this type of technology due to increasing demand.
Researchers and companies continue to make smaller and more lightweight robotic surgery prototypes, along with new training programs for safer surgeries. Over the years, robotic surgery systems have become more streamlined and comfortable for doctors to use and the technology that powers these systems continues to improve. They have upgraded features like near-infrared technology and enhanced 3D cameras, which supply views that are magnified by 10 times.
Why choose us?
Dr Kriplani is a high volume laparoscopic and colorectal surgeon and considered pioneers in this kind of surgery with decades of experience and continuously meets the highest quality benchmark. We use the latest diagnostic and treatment options. We avoid colostomy in a high percentage of patients because of our experience, skills and sophisticated tools.
Besides diverticular disease and colorectal cancer we also treat a wide variety of Colorectal diseases which include.
- Inflammatory bowel diseases (IBD) like Crohn’s disease and ulcerative colitis
- Rare tumors of the small and large bowel like Neuro-endocrine (carcinoid) tumors, gastrointestinal stromal tumors (GIST), Presacral tumors, Appendiceal neoplasms, Small intestinal adenocarcinoma, Mesenteric fibromatosis
- Benign anorectal diseases. Haemorrhoids, anal fistula, abscess, anal fissure,
- Enteric fistulas Enterocutaneous fistulas, Colocutaneous fistulas
- Functional bowel disorder. Slow transit constipation, rectal prolapse, Rectovaginal fistula, faecal incontinence, Sphincter injury, pelvic floor dysfunction.