Haemorrhoids surgeries
Haemorrhoids, commonly known as piles, are swollen and inflamed veins in the rectum and anus that cause discomfort and bleeding. They can be classified into internal haemorrhoids, which occur inside the rectum, and external haemorrhoids, which develop under the skin around the anus. Factors such as chronic constipation, straining during bowel movements, and prolonged sitting can contribute to their development. Treatment options range from lifestyle modifications and over-the-counter remedies to minimally invasive procedures and surgical interventions, depending on the severity and persistence of symptoms.
Haemorrhoids
What are Haemorrhoids ?
Internal Haemorrhoids
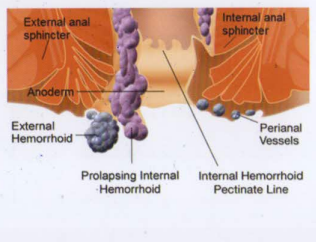
Internal haemorrhoids are located in the inside lining of the rectum and cannot be felt unless they are substantially enlarged. They usually are painless and make their presence known by causing bleeding with a bowel movement. Sometimes internal haemorrhoids prolapse or protrude outside the anus. If so, you may be able to see or feel them as moist pads of skin that are more pink than the surrounding area. Prolapsed haemorrhoids may hurt because the anus is dense with pain-sensing nerves. Prolapsed haemorrhoids usually recede into the rectum on their own: if they don’t, they can be gently pushed back into place.
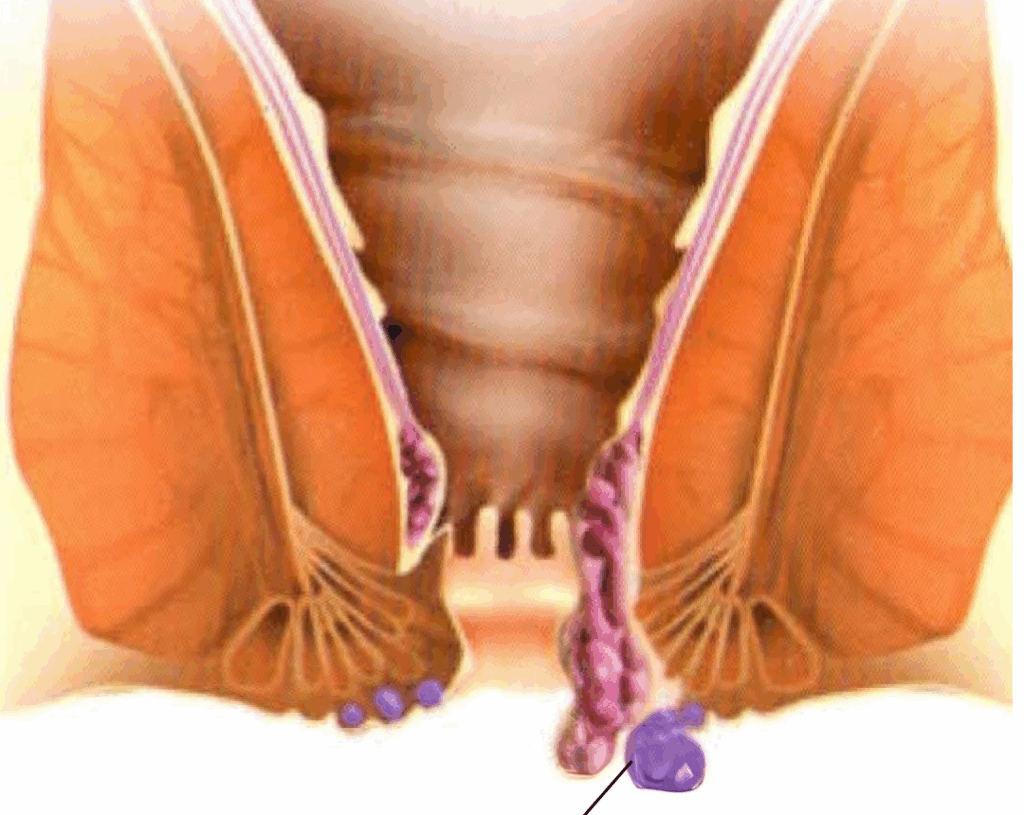
External Haemorrhoids
External haemorrhoids are located underneath the skin that surrounds the anus (lower in the anus than internal haemorrhoids). They can be felt when they swell, and may cause itching, pain, or bleeding with a bowel movement. If an external haemorrhoid prolapses to the outside (usually in the course of passing a stool), you can see and feel it. Blood clots sometimes form within prolapsed external haemorrhoids, which can cause an extremely painful condition called thrombosis. If an external haemorrhoid becomes thrombosed, it can look rather frightening, turning purple or blue, and could possibly bleed. Despite their appearance, thrombosed haemorrhoids usually are not serious though they can be very painful. They will resolve on their own in a couple of weeks. If the pain is unbearable, the blood clot can be removed from the thrombosed haemorrhoid, which stops the pain.
WHAT CAUSES HAEMORRHOIDS?
It is not certain what causes haemorrhoids. It is likely, that extreme abdominal pressure causes the veins to swell by blocking the flow of blood through them. They then become susceptible to irritation. The increased pressure can be caused by obesity, pregnancy, standing or sitting for long periods, straining on the toilet, coughing, sneezing, vomiting, and holding your breath while straining to do physical labor.
WHAT IS THE ROLE OF DIET IN HAEMORRHOIDS?
Diet is believed to have a pivotal role in causing/ preventing haemorrhoids. People who consistently eat a high-fiber diet are less likely to get haemorrhoids, while those people who prefer a diet high in processed foods are at higher risk. A low-fiber diet or inadequate fluid intake can cause constipation, which can contribute to haemorrhoids in two ways:
- It promotes straining on the toilet; and
- It also aggravates the haemorrhoids by producing hard stools that further irritate the swollen veins.
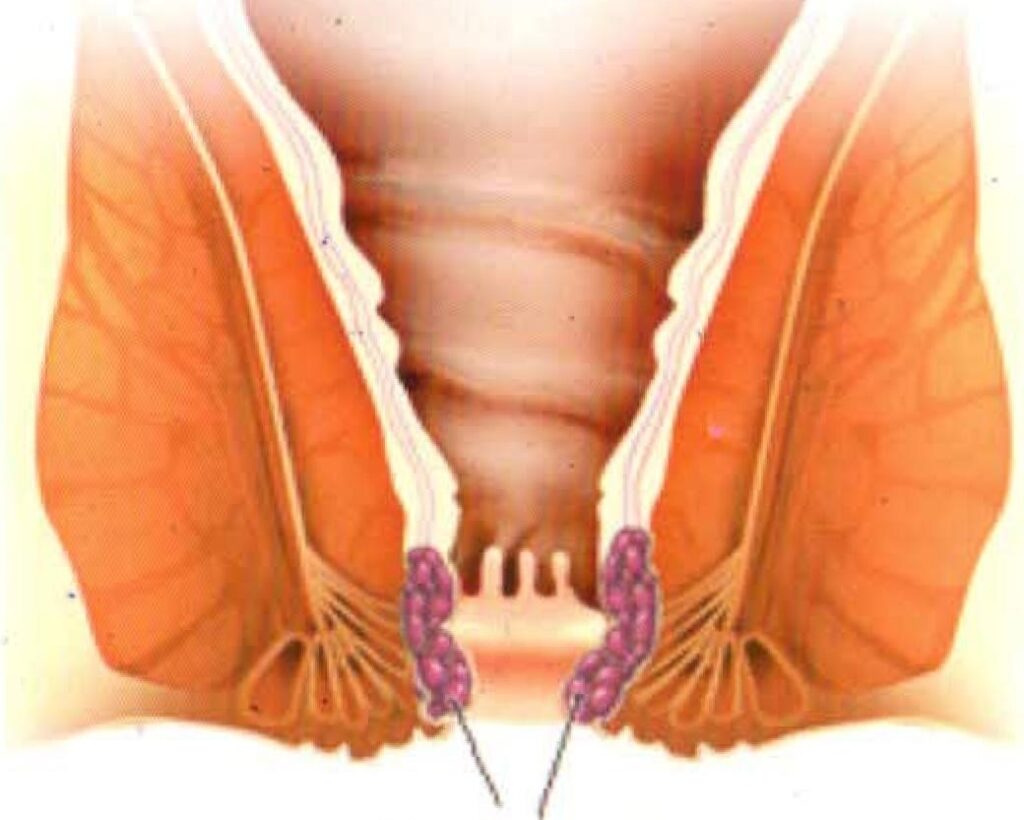
Internal Haemorrhoids
External Haemorrhoids
What are the grades of Haemorrhoids?
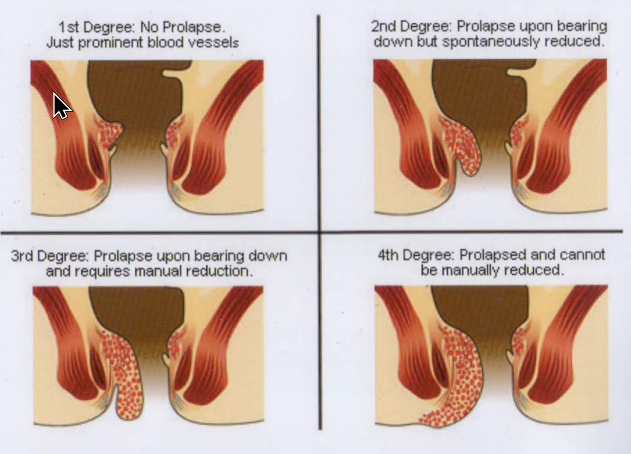
First-degree haemorrhoids: Haemorrhoids that bleed, but do not prolapse out.
Second-degree haemorrhoids: Haemorrhoids that prolapse out and retract on their own (with or without bleeding).
Third-degree haemorrhoids: Haemorrhoids that prolapse out but do not retract on their own . They must be pushed back in by a finger.
Fourth-degree haemorrhoids: Haemorrhoids that prolapse and cannot be pushed back in the anal canal. Fourth-degree haemorrhoids also include haemorrhoids that are thrombosed (containing blood clots) or that pull much of the lining of the recturm through the anus.
Treatment
Haemorrhoids. are treated with a variety of measures including, diet, over-the-counter medicine (creams, lotions, gels, pads, wipes, etc.), procedures (sclerotherapy, rubber band ligation, etc.) and surgery(open sugery, stapled surgery and LASER surgery).
WHAT ARE THE SYMPTOMS OF HAEMORRHOIDS?
The most common symptom and sign of haemorrhoids is painless bleeding. There may be bright red blood on the outside of the stools, on the toilet paper, or dripping into the toilet, The bleeding usually is self-limiting. Bleeding with a bowel movement is never normal and should prompt a visit to a doctor While haemorrhoids are the mast common cause of bleeding with a bowel movement, there may be other reasons to have bleeding including inflammatory bowel disease, infection, and tumors.
WHAT ARE THE SYMPTOMS OF PROLAPSED HAEMORRHOIDS?
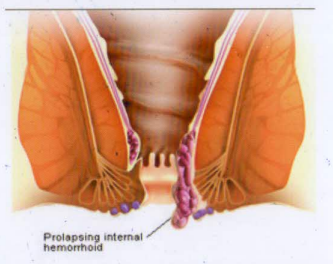
Prolapse of an internal haemorrhoid occurs when the internal haemorrhoids swell and extend from their location in the rectum through the anus. In the anal canal, the haemorrhoid is exposed to the trauma of passing stool, particularly hard stools associated with constipation. The trauma can cause bleeding and sometimes pain when stool passes. The presence of stool, inflammation, and constant moisture can lead to anal itchiness (pruritus ani), and occasionally the constant feeling of needing to have a bowel movement. The prolapsing haemorrhoid usually returns into the anal canal or rectum on its own or can be pushed back inside with a finger, but it prolapses again with the next bowel movement.
WHAT ARE THE SYMPTOMS OF THROMBOSED EXTERNAL HAEMORRHOIDS?
External haemorrhoids can be felt as bulges at the anus, but they usually cause few of the symptoms that are typical of internal haemorrhoids. External haemorrhoids can cause problems, however, when blood clots inside them. This is referred to as thrombosis. Thrombosis of an external haemorrhoid causes an anal lump that is very painful and tender, and often requires medical attention. The thrombosed haemorrhoid may heal with scarring, and leave a tag of skin protruding in the anus. Occasionally, the tag is large, which can make anal hygiene (cleaning) difficult or irritate the anus.
HOW ARE HAEMORRHOIDS DIAGNOSED?
Most individuals who have haemorrhoids discover them by either feeling the lump of an external haemorrhoid when they wipe themselves after a bowel movement, note drops of blood in the toilet bowl or on the toilet paper, or feel a prolapsing haemorrhoid (protruding from the anus) after bowel movements. By the history, the physician can suspect haemorrhoids which can be diagnosed on the basis of a careful examination of the anus and anal canal.
Rectal examination with a gloved finger may uncover an internal haemorrhoid high in the anal canal. The rectal examination is more helpful in excluding rare cancers that begin in the anal canal and adjacent rectum. A more thorough examination for internal haemorrhoids is done visually using an anoscope. Whether or not haemorrhoids are found, if there has been bleeding, the colon above the rectum needs to be examined to exclude other important causes of bleeding other than haemorrhoids such as colon cancer, polyps, and colitis.
HOW ARE GRADE I AND GRADE II HAEMORRHOIDS TREATED?
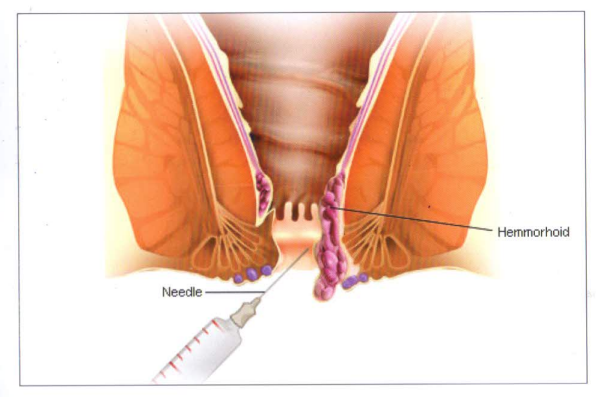
Grade I & II haemorrhoids are treated in the out-patient department as follows:
- Haemorrhoid Treatment – Diet
It is recommended that individuals with haemorrhoids soften their stools by increasing fiber in their diet. Fiber is found in numerous foods including fresh and dried fruits, vegetables, grains, and cereals. Generally, 20 to 30 grams of fiber per day is recommended. Stool softeners and increased drinking of liquids also may be recommended. lsapgol husk and fruits with their skins help in forming bulk in the stool and are natural laxatives. - Haemorrhoid Treatment Through Medication
Products used for the treatment of haemorrhoids are available as ointments, creams, gels, suppositories, foams. Ointments, creams, and gels, when used around the anus, should be applied as a thin covering. When applied to the anal canal, these products should be inserted with a finger. - What is Warm Sitz Baths in Haemorrhoid Treatment?
Sitting in a few inches of warm water with 10 drops of povidone-iodine solution (Betadine) three times a day for 10-15 minutes (sitz bath) helps decrease the inflammation of the haemorrhoids. It is important to dry off the anal area completely using a soft clean towel after each sitz bath to minimize irritation of the skin surrounding the anus. - Haemorrhoid Treatment- Stool Softeners
Stool softeners may help, but once haemorrhoids are present, even liquid stools may cause inflammation and infection of the anus. Discuss with yon doctor regarding their use. - Haemorrhoid Treatment- Sclerotherapy
This therapy is usually used for Grade I & II haemorrhoids. Sclerotherapy is one of the oldest & most effective forms of treatment for haemorrhoids. During sclerotherapy, a liquid (5% phenol in oil) is injected into the base of the haemorrhoid. The veins thrombose and scarring takes place. Pain and mild bleeding may occur during sclerotherapy which usually subsides in 2-3 days. A repeat session of the procedure is needed after 3 weeks. With two sessions, 90% of grade I & II haemorrhoids subside Symptoms of haemorrhoids may return after several years and may require surgery.
WHAT IS THE TREATMENT OF GRADE III / GRADE IV HAEMORRHOIDS?

Surgical removal of haemorrhoids known as a haemorrhoidectomy or stapled haemorrhoidectomy is reserved for patients with third or fourth degree haemorrhoids.
Haemorrhoidectomy
During a haemorrhoidectomy, the internal haemorrhoids and external haemorrhoids are cut out. The wound left by the removal is left open. Postsurgical pain is a major problem with haemorrhoidectomy, and potent pain medications (narcotics) usually are required. The open wound needs daily dressings and takes about 3-4 weeks to heal completely.
What is Stapled Haemorrhoidectomy (Minimally Invasive Procedure for Haemorrhoids MIPH)?
A newer surgical technique is rapidly becoming the treatment of choice for third-degree haemorrhoids. This surgery removes the expanded haemorrhoidal supporting tissue that has allowed the haemorrhoids to prolapse downward. In this procedure, a circular, hollow tube is inserted into the anal canal and a suture (a long thread) is placed through it and woven circumferentially within the anal canal above the internal haemorrhoids. The ends of the suture are brought out of the anus through the hollow tube. The stapler is placed through the hollow tube and the ends of the sutures are pulled expanding the haemorrhoidal supporting tissue into the jaws of the stapler. The haemorrhoidal cushions are pulled back up into their normal position within the anal canal. The stapler is then fired, cutting off circumferential ring of expanded haemorrhoidal supporting tissue trapped within the stapler, at the same time stapling together the upper and lower edges of the cut tissue. Stapled haemorrhoidectomy is less painful and faster than a traditional haemorrhoidectomy, taking approximately 15-20 minutes.
The difference in the pain as compared to the open Haemorrhoidectomy is very significant. Also, there is no wound and hence the discomfort of daily dressing is done away with. The blood loss is minimal (usually <5-10 ml) in MIPH and the patient can be ambulated very rapidly, regaining normal routine and activities in 3-5 days.
Occasionally associated skin tags are present which regress on their own. Certain patients request removal of these tags and once removed, the raw area can pain for 3 days to 2 weeks.
WHAT IS LASER TREATMENT OF HAEMORRHOIDS?
For treatment of piles or haemorrhoids, a fine LASER beam is directed into the haemorrhoids, which are swollen and inflamed anal lining and vascular cushions, to cause shrinking. This is done by using a LASER generator and optical fiber, to focus a narrow beam of light, that disrupts the abnormal blood flow in these tissues. LASER surgery for piles is usually performed as a single day procedure where the patient can be discharged within 24 hours under regional anesthesia / general anaesthesia. Only after a thorough examination, the best procedure for the patient can be decided. LASER treatment is most suited for grade II and grade III haemorrhoids. For grade IV haemorrhoids LASER is not so suitable. Sometimes a combination of procedures may be advised e.g. MIPH with ligasure excision for grade IV haemorrhoids, MIPH / lateral sphincterotomy if an associated fissure is present or Laser with Haemorrhoidal artery ligation (HAL).
- Less postoperative pain.
- Minimal blood loss and least tissue loss.
- Small wounds that do not require closure.
- Early return to work.
WHAT CARE IS NEEDED AFTER THE SURGERY?
After the procedure, the patient is shifted to a recovery room for post-operative monitoring of vitals whilst regaining consciousness until the anesthesia wears off and breathing becomes normal. During this time, slight discomfort and likely minimal pain at the surgical site is expected for which intravenous analgesics are prescribed.
The care following Haemorrhoidectomy is fairly simple. It is common to have burning sensation, discomfort and mild pain for 1 -3 days after surgery. These can be minimized by:
- Take warm water sitz bath after each bowel movement for 10 min using 8-10 drops of povidone iodine solution.
- Apply Lignocaine 2% gel in the anus before and after passing stools and at night
- Laxative has to be taken for atleast a week after surgery and straining while passing stools should be avoided.
- Constipation has to be strictly avoided as it is the main cause for recurrence.
- Anti-inflammatory drugs have to be taken for 3-5 days.
- Usually no dressings are required unless specified by your doctor.
The night after surgery high fiber diet is started. Patients can go home in a day or two
HOW CAN I ENSURE FAST RECOVERY?
The outcome of every treatment largely depends on what the patient does to ensure the best healing. After haemorrhoid surgery, the cure depends on specific measures in individual care and precautions as prescribed by the surgeon.
These include:
- Keeping the area clean and dry most of the time. Use a sanitary napkin or diaper after sitz bath.
- Taking precautions against constipation, in the form of adequate water intake and roughage. Mild exercise/activity helps with constipation.
- Regular wash when recommended with saline and dilute Hydrogen peroxide.
- Regular review in the post-operative period till the wound heals completely.
- Optimal treatment of other medical conditions
Don’ts:
- Avoid straining at stools.
- Avoid lifting or pulling weights or exert too much pressure on the body or indulge in strenuous physical activity for atleast two weeks.
- Don’t go sedentary. Keep moving and walking.
- Avoid outside (oily fried) foods.
HOW CAN WE PREVENT HAEMORRHOIDS?
The best way to prevent haemorrhoids is to keep your stools soft so they are easy to pass and don’t require straining. Eating a high-fiber diet and drinking plenty of fluids (six to eight glasses each day) can help you stay regular and your stools soft, and may reduce constipation and the need to strain on the toilet, lowering your risk of developing new haemorrhoids.